Many of the foods we eat can irritate and damage the very delicate and critically important digestive system in our bodies, which can in turn lead to anything from inflammation in the gastrointestinal tract to an immune response. Even nutrient absorption can be affected. One such food is wheat, which contains gluten.
What is gluten?
Gluten is a protein found in foods processed from wheat and similar cereals, including barley, spelt and rye. It contains gliadins and glutenins, the two main components of the gluten fraction of wheat seeds. Both are known intestinal irritants. Gluten is primarily used in modern food processing to give elasticity to dough, helping it to rise and to keep its shape, and often giving the final product a chewy texture. Greater refinement of the gluten leads to chewier products, while less refinement yields softer baked goods. One of the most common ways that we now take in carbohydrates is through grains in our diet, especially wheat. It is a staple food, with 600 million tonnes eaten every year. On average, it makes up roughly half of the calorie intake of a person’s diet. Unfortunately, gluten constitutes 78% of the total protein in modern wheat. What this means in practice is that gluten sensitivities and allergies are extremely common. In fact, it is thought that as many as 1 in 10 people are sensitive to gluten, while coeliac disease (an autoimmune condition related to gluten intake) affects almost 1 in 100 people.

Gluten sensitivity
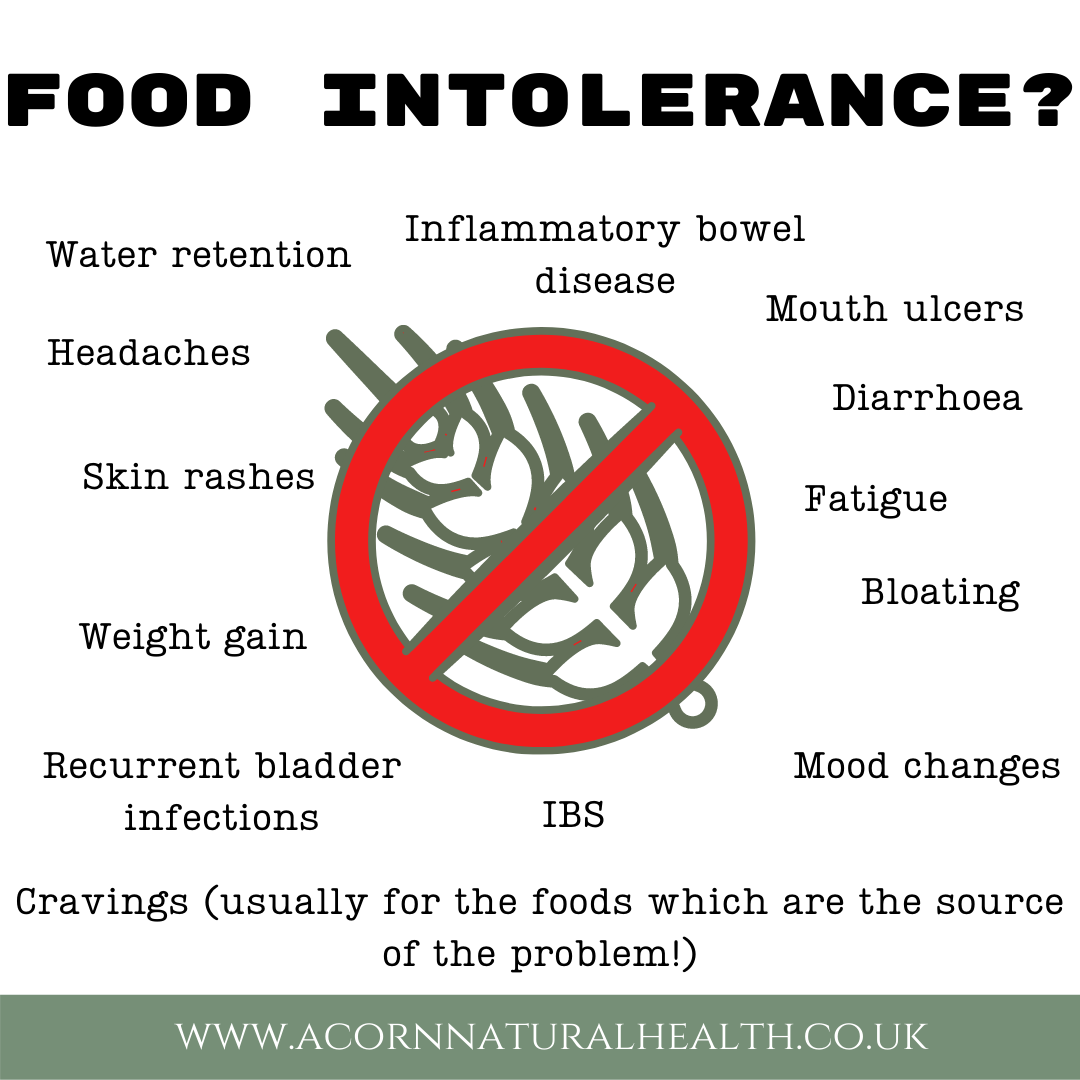
Often, people with a sensitivity to gluten have no digestive symptoms at all. This can make diagnosis very difficult, and may also mean that appropriate dietary changes are not made by the sufferer. Where symptoms are present, some of the most common include:
- bloating
- diarrhoea
- constipation
- diverticulitis
- digestive problems, even as drastic as Crohn’s disease
- fatigue
- upper respiratory tract problems (such as sinusitis and ‘glue’ ear)
- depression
- and behavioral problems in children (such as ADHD).
Of all the grains causing gluten sensitivities, wheat is the number one culprit. Gluten sensitivity is not a food allergy; it is a condition of the gut. After eating gluten-foods, undigested gluten proteins resting in the intestines are treated by the body like an invader, resulting in irritation of the gut and the flattening of the microvilli (finger-like protrusions that run along the intestinal walls). Without the microvilli, there is far less surface area with which to absorb nutrients from food. This is why those with gluten sensitivities can sometimes experience symptoms of malabsorption, such as chronic fatigue, nutrient deficiencies, anaemia, osteoporosis, nausea, skin rashes, depression and more. If gluten is eliminated from the diet, the gut usually heals and the symptoms disappear over time. This is therefore usually the recommended course of action, along with supporting supplementation (see below).
Coeliac disease
Unlike a gluten sensitivity, coeliac disease involves an abnormal immune reaction to partially digested gliadin. Coeliac disease is neither a food allergy nor an intolerance – it is an autoimmune disease. The body’s immune system attacks itself when gluten is eaten. This can cause serious and lasting damage to the lining of the gut and may mean that the body is unable to properly absorb nutrients from food. Symptoms of coeliac disease range from mild to severe bloating, excessive flatulence, diarrhoea, constipation, abdominal cramps, fatigue, aches and pains, flu-like symptoms, and/or mood swings. It is now recognised as one of the most common chronic health disorders in Western countries, yet it is still one of the most under-diagnosed. As the symptoms are so broad, they can be attributed to a wide range of other health conditions. As such, coeliac disease is often misdiagnosed as, for instance, fibromyalgia, lupus, multiple sclerosis, chronic fatigue, irritable bowel syndrome and Crohn’s disease.
Up until about a decade ago, most medical experts believed that coeliac disease was relatively rare and only affected about 1 in 2,500 people. It was also thought to be a disease that primarily affected children and young people. More recent studies, along with advances in diagnosis, have shown that the condition is much more prevalent.
Addressing the underlying problem
Gluten sensitivity can be one of the symptoms of a leaky gut syndrome. It is no surprise that when the lining of the intestines becomes more permeable, it can lead to a problem with many food sensitivities. Gluten (and dairy!) is very commonly encountered ‘maintaining cause’ in the digestive problems I see in my clinic. It is always worth looking back to determine what could have contributed to the body becoming more sensitized to particular food items- did it start after prolonged stress? Bouts of sore throats? Series of antibiotic treatments? Although removing gluten from the diet is always beneficial in such cases, it’s equally important to support the body in ‘sealing’ the damage which might have been contributing to unpleasant symptoms for even a number of years. Addressing the ‘root cause’ of the problem (whether it’s stress management or rebalancing the aftermath of antibiotic or steroid treatment) will help your body build resilience and minimise chances of a relapse.
Extra support for a gluten-free gut
As with a gluten sensitivity, coeliac disease is usually treated by simply adopting a gluten-free diet, i.e. excluding all foods that contain gluten. This is a permanent step in the case of coeliac disease, and usually recommended to be permanent in the case of gluten sensitivity- although it doesn’t have to be. A gluten-free diet is an effective means of preventing damage (or at least further damage) to the lining of the intestines and avoiding the associated symptoms of both conditions, even if such approach doesn’t address the problem in itself. And these days, maintaining a gluten-free diet isn’t the hardship it was even ten years ago. If you are happy to focus on only eliminating gluten out of your diet, there are now whole dedicated areas of most large supermarkets and health stores for “free from” ranges. However, as with any restricted diet, it is important to continue to ensure a balanced diet and the intake of a broad spectrum of nutrients. Given the reduced number of food choices, this can sometimes be a challenge, particularly in the early days. But careful meal planning will help, along with opting for seasonal, preferably organic food. In addition, many people with a gluten sensitivity or coeliac disease choose to supplement their diets for extra support, both in terms of nutrient intake and for digestive health. This can be particularly helpful where the gut is irritated and inflamed from years of gluten exposure. Multi-strain probiotics (beneficial bacteria), prebiotics (food for beneficial bacteria), Omega oils and the amino acid glutamine are particular favourites for supporting a healthy gut, lower levels of inflammation, along with gut wall integrity. What’s more, many of the better food and dietary supplements will also be gluten-free.